the operating room

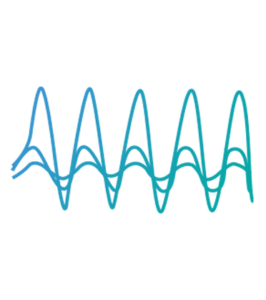
SSEP
Somatosensory Evoked Potentials (SSEP) assess brain and spinal cord function. Electrical stimulation applied to the upper and lower extremities initiate activity along peripheral nerves, up the posterior column of the spinal cord, and through the brainstem to the sensory cortex of the brain. SSEP are recorded with subdermal electrodes strategically placed to detect responses from neural generators along the sensory pathway. Absence of the expected response, delays in transmission time, or alteration of the waveform can indicate specific areas of concern.

EMG
Electromyography (EMG) uses muscle activity to identify and prevent damage to structures in the nervous system. EMG is typically recorded with subdermal needle electrodes placed in the target muscles, selected based on the surgical procedure. Spontaneous or free run EMG can help to prevent postoperative nerve damage from surgical manipulation. Triggered EMG, on the other hand, requires a stimulus. With in-situ stimulation, the surgeon can identify specific nerve roots, peripheral nerves, cranial nerves, or test for nerve root impingement after pedicle screw placement.
MEP
Motor Evoked Potentials (MEP) provide selective and specific assessment of the functional integrity of descending motor pathways, from the motor cortex to peripheral muscles. Using transcranial electrical stimulation, MEP monitor motor function of the cortex and anterior spinal cord by recording compound muscle action potentials (CMAP) from muscles. MEP are recorded with subdermal needle electrodes from target muscles. These target muscles are selected based on the surgical procedure and spinal levels involved. Changes in MEP are useful for evaluating early ischemic or mechanical damage to the spinal cord. A significant decrease in the amplitude of muscle MEP, although not always associated with postoperative neurological deficit, are considered alarm criteria.
BAER
Brainstem Auditory Evoked Responses (BAER) monitor the auditory pathway from the cochlea through the brainstem. A rapid series of clicks are delivered to the ear using special intraoperative transducers placed in the ear canal, and responses are recorded as they travel from the cochlea to the auditory nerve and then through the brainstem assessing the integrity of the nerve and brainstem structures.

EEG
Electroencephalography (EEG) is used to compare side-to-side hemispheric differences in cerebral perfusion as well as global electrical brain activity alterations. EEG is recorded via subdermal needles electrodes placed in the scalp according to the International 10/20 System.
Transcranial Doppler
Transcranial Doppler ultrasound measures blood flow through major vessels of the brain using a probe placed on specific areas of the skull to maximize insonation of the studied vessel. This non-invasive technique can determine if adequate blood flow is maintained, reduced, or blocked.
Micro-doppler
Micro-Doppler sonography confirms patency and blood flow through arteries and veins intraoperatively. Surgeons can assess whether blood is moving towards or away from the probe, along with its relative velocity, using a sterile 20MHz handheld probe within the surgical field.